In the first three parts of this series, I made the case for electronic health records, addressed their problems, and then talked about the need to build structures to share this data with one another to improve care and lower costs.
I believe we are on the cusp new technologies for medical screening with recent advances in innovations around:
- Natural language processing;
- Machine learning with neural networks; and
- The immense affordable storage available on the cloud.
These could allow for the EHR, as we understand it, to become obsolete.
Instead, a physician could examine a patient and, via voice recognition, NLP could transcribe the note to a database immediately. This would free the physician and patient to form the therapeutic bond that is vital to improved understanding and outcomes.
Equally important, intelligent decision support embedded in a physician’s computer would allow for more timely and accurate diagnosis and treatment.
Imagine a new type of computer listening to patient describe their symptoms. This computer would already have the data from prior visits such as the medications, allergies, history and active medical problems. The computer could access all the current knowledge regarding diagnosis and treatment of any medical disorder and provide the physician with a differential diagnosis and the best evidenced treatment plan.
In fact, it could enable predictive care that results in early diagnosis and reduced mortality rate.
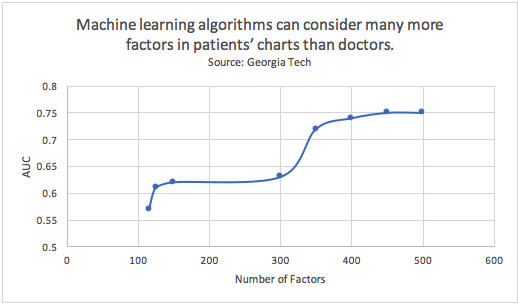
Consider death from congestive heart failure (CHF) and related complications. Research from Georgia Tech has shown that machine-learning algorithms can evaluate far more factors in patients’ records than physicians can alone. As a result, machine learning significantly increases the system’s ability to accurately discern people who have CHF from those who don’t.
Predictive modeling over data derived from EHRs is being used for early diagnosis and is reducing mortality rates from problems such as congestive heart failure and sepsis. Congestive Heart Failure (CHF) accounts for the most health care spending. The earlier it is diagnosed the better it can be treated avoiding expensive complications, but early manifestations can be easily missed by physicians. A machine learning example from Georgia Tech demonstrated that machine-learning algorithms could look at many more factors in patients’ charts than doctors, and by adding additional features there was a substantial increase in the ability of the model to distinguish people who have CHF from people who don’t.
Coupled with information about a physician’s total population of patients, all of this would allow us to understand how the individual patient’s outcome compares to the norm – and that could revolutionize healthcare for the better.
We already see glimpses of this with creative organizations displaying the overall Hemoglobin A1c average for a physician’s total diabetic patient population.
This reference allows for the physician and patient to comprehend how the individual patient’s outcome differs from the norm. Imagine a physician coming work in the morning with a dashboard of information about his/her patient’s displayed on the EHR screen.
Smart algorithms would have discovered that 25% of the patients have undiagnosed depression and that this factor triples the cost of care for patients with diabetes, shortens the lifespan of patients with CHF and causes unneeded misery for a quarter of his patients.
It is time we use all the resources to improve the healthcare of our patients.
It is time that we introduce disruptive innovations into the mix for the sake of our patients and the financial stability of our system.

